in Frail Older People
In Australia, almost 1 in 4 older adults aged 65 years and over suffer from chronic pain
Chronic non-cancer pain is a common problem among older people and has a significant impact on their quality of life. Medical comorbidities and polypharmacy are often additional challenges in managing these patients. Appropriate assessment of chronic non-cancer pain is important for the development of a patient-centered, goal-directed management plan.
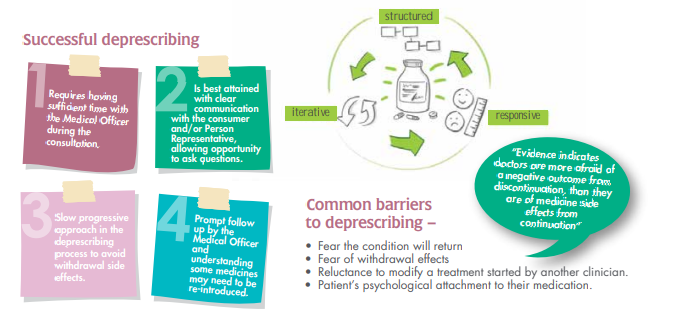
When assessing patients with cognitive impairment, modified communication strategies and validated pain assessment tools can be useful. The quantity and quality of the evidence supporting individual drugs in the management of chronic non-cancer pain varies and studies focused on frail older people are limited. Caution is generally advised when introducing drugs and escalating the doses. Drugs that are not effective should be stopped. A shared decision-making approach is advised for deprescribing analgesics used for chronic non-cancer pain
Let’s define Chronic Non-Cancer Pain
Chronic non-cancer pain is defined as pain lasting beyond the time of tissue healing or for over three months. It is a significant problem among older people, due to the high prevalence of conditions, such as osteoarthritis, in which pain is a predominant symptom.
Older people living with chronic pain are more likely to report significant limitation in their daily
activities as compared to those without chronic pain. Chronic non-cancer pain can have a negative impact on a person’s psychological well-being, and vice versa.
However, it is under-recognised, undertreated, and often challenging to manage. The presence of
frailty in older people adds an extra layer of complexity, given these patients often have several
comorbidities treated with multiple medicines and are prone to falls and adverse effects.
Assessment
The first step in the successful management of chronic non-cancer pain is recognising the presence of pain and accurately assessing its severity and impact on function, in conjunction with history and examination.
Stoicism, and the expectation that pain is part of aging, have been implicated in the under-reporting of
pain in older people.
Cognitive and sensory impairments that affect communication can also limit the accurate identification of
pain. The initial assessment needs to identify or exclude serious and treatable causes of pain, before
embarking on a symptom management approach.
In a holistic assessment, it is important to address the psychological and functional impact of chronic
non-cancer pain.
Multiple functional assessment tools are validated and practical for use in older people. Understanding
the impact of the pain can facilitate negotiating realistic and meaningful treatment goals. For example, in
some cases improving self-care or mobility to enable the person to participate in certain life activities will
be more achievable than complete pain relief.
Pain assessment in older people
• Provide adequate time to discuss their pain, process the question, and to formulate a response.
• Use open-ended questions when discussing pain, rephrase the questions to elicit the presence of pain,
for example:
Do you hurt anywhere?
Do you have any aches, soreness, or discomfort?
What is stopping you from doing what you want to do?
• Use a self-reported pain measurement tool to assist in evaluation e.g. brief pain inventory.
• Arrange for someone who knows the patient well to do the pain assessment and use the same tool and standardised wording during each discussion.
It is important to include insights and observations from family members and familiar carers about behaviour that may be pain related. When reassessing the efficacy of pain management, the same scale should be used each time.
Drug treatment

Drugs only form part of a multidimensional management plan for chronic non-cancer pain, in conjunction with other strategies, such as physical exercise and cognitive behavioural therapy.
When a decision is made to prescribe, careful
consideration should be taken off the age-related
physiological changes and the impact of polypharmacy in older people.
Current guidelines recommend the following general principles when prescribing for older people:
• Start one drug at a time, at a low dose, with slow-dose titration.
• Allow an adequate time interval to enable the drug to take effect, before introducing additional drugs.
• Constantly monitor efficacy and adverse effects and adjust or cease the drug if required.
• Consider deprescribing at regular intervals once self-management of pain is achieved.
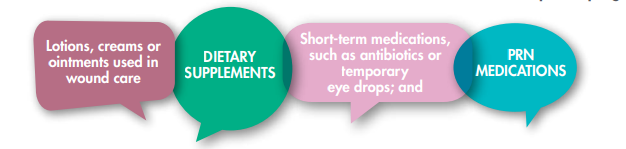
• Review all analgesia, including over-the-counter products, for potential interactions.
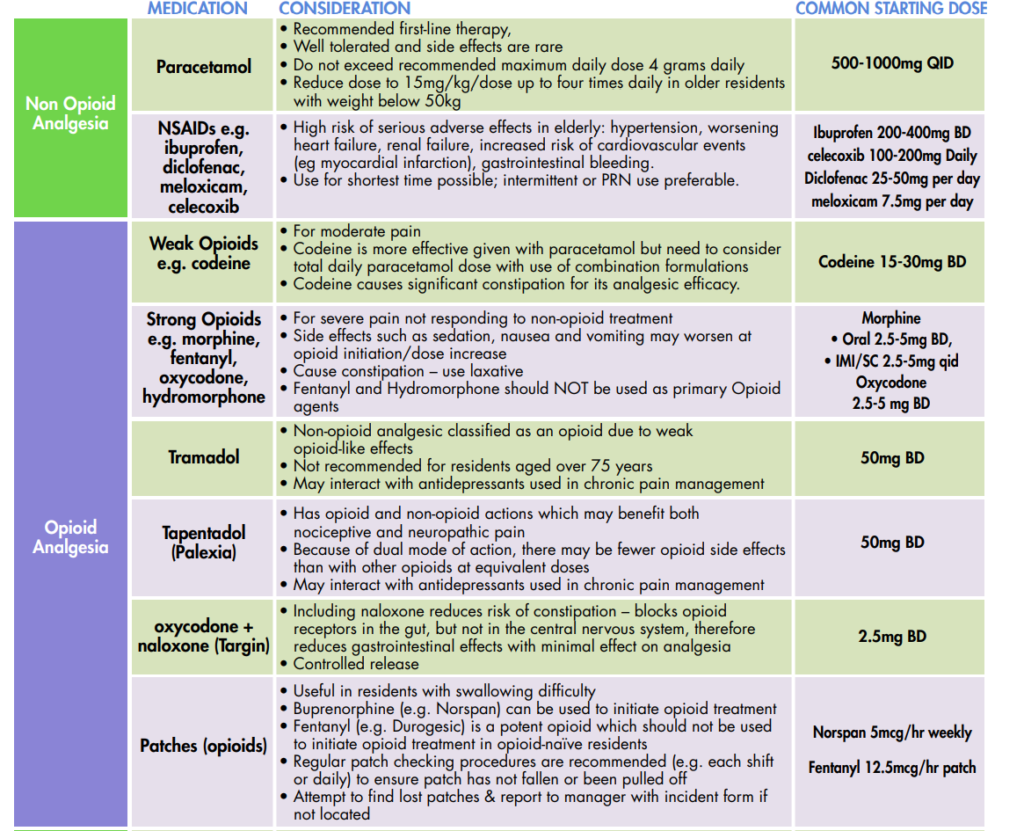
Analgesic dosing considerations in frail older people with chronic non-cancer pain
Paracetamol
Although paracetamol is the first-line analgesic, particularly for non-Cancer pain, its efficacy is modest. Evidence supporting its long-term use is limited, but it remains in multiple guidelines as the first-line drug, especially for older people, given that other options are often contraindicated.
In view of an increased risk of hepatotoxicity in older adults, sometimes at therapeutic doses, and emerging evidence of a relative lack of efficacy of paracetamol, the benefits of long-term use need to be re-evaluated particularly when combined with other analgesics due to ongoing reports of pain.
The use of paracetamol for a limited duration is recommended with a review of the response to therapy and discontinuation if there is no response.
NSAID
The gastrointestinal, renal and cardiovascular adverse effects of NSAIDs are well known. Upper gastrointestinal
complications occur in 1% of older patients treated for 3–6 months and in 2–4% of those treated for one year.
This risk continues with longer durations of use.
The efficacy of NSAIDs for knee osteoarthritis diminished
and lost clinical significance after eight weeks of therapy.
International guideline recommendations do not exclude
using NSAIDs in very old people for some musculoskeletal pains, however, they are only recommended for short-term treatment of up to 6 weeks.
Co-administration with a proton pump inhibitor is advised for patients at risk of gastrointestinal complications, including the history of ulcers and concomitant use of certain drugs (anticoagulants or antiplatelet drugs, including low-dose
aspirin). Topical NSAIDs may be a safer alternative for localised pain. They are the preferred treatment for pain associated with osteoarthritis in the hands and knees
DOSING CONSIDERATIONS
Decreased volume of distribution (20%) and clearance (37%) in frail older people, hence guidelines recommend reduced doses:
• 0.5–1 g every four to six hours, up to a maximum of 3 g in 24 hours, if weight >50 kg
• 15 mg/kg/dose every four to six hours up to a maximum of four doses in 24 hours, if weight <50 kg.
DOSING CONSIDERATIONS
Increased prevalence of chronic renal disease and co-prescription of
anticoagulation and antiplatelet therapies in frail older people makes this class of analgesics discouraged.
Consider dose reduction and co-administration of proton pump inhibitors if indicated.
Adjuvant Drugs
In chronic non-cancer pain with a neuropathic component, there is evidence supporting the use of adjuvant drugs, such as gabapentin, tricyclic antidepressants and selective serotonin noradrenaline reuptake inhibitors.
These drugs have been recommended as first-line therapy based on a meta-analysis of moderate- to high-quality trials in post-herpetic neuralgia and diabetic neuropathy.
However, these trials did not specifically involve older
people, so caution is advised when prescribing these drugs in frail older patients, and tricyclic antidepressants are not advisable given the high risk
of adverse effects
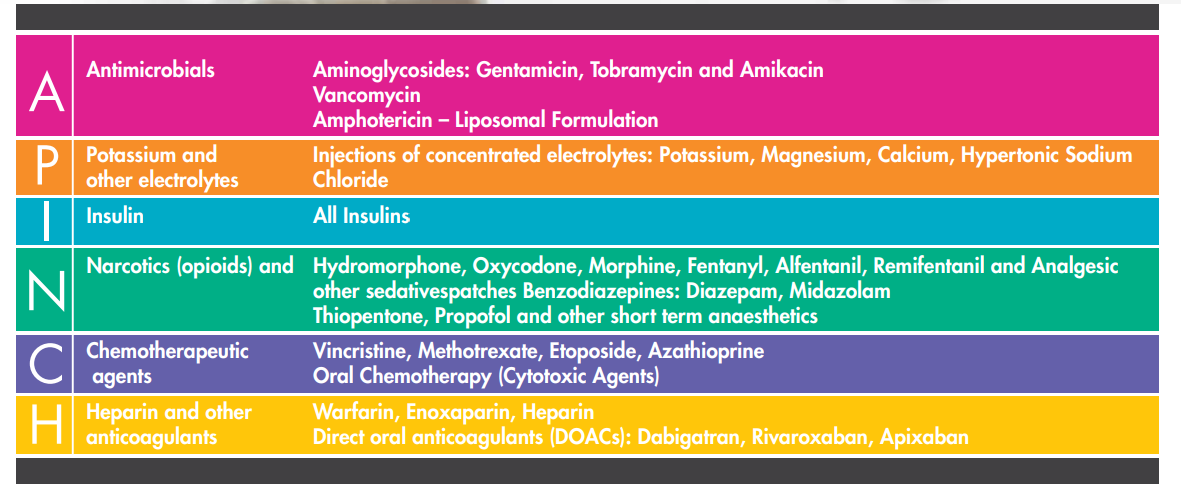
Opioids
Current guidelines do not support the long-term use of
opioids in chronic non-cancer pain. There is a lack of
evidence for long-term efficacy, but significant evidence of harm. A recent meta-analysis of 30 studies associated opioid use with falls, fall injuries and fractures in older people.
Opioids are therefore not recommended other than in
exceptional circumstances when other treatments have failed and the pain has been shown to be opioid-responsive. High doses and co-administration with benzodiazepines should particularly be avoided in frail older people given the additional risk of harm.
Data on the use of newer opioids, such as tapentadol, for
chronic non-cancer pain is limited and although tolerability of sustained-release tapentadol in patients aged 75 years or older showed a more favourable adverse-effect profile than conventional opioids, neurological and psychiatric adverse effects were higher than traditional opioids in frail older nursing home patients with dementia, especially those using
antidepressants
DOSING CONSIDERATIONS
Adverse reactions such as sedation and anticholinergic
effects limit use.
Reduce starting dose and slow up-titration with close
monitoring in frail older people and those with renal or
hepatic impairment.
DOSING CONSIDERATIONS
Increased risk of falls and subsequent fractures, delirium
and excessive sedation in older people.
The additional risk associated with high-dose use and
co-administration with benzodiazepines
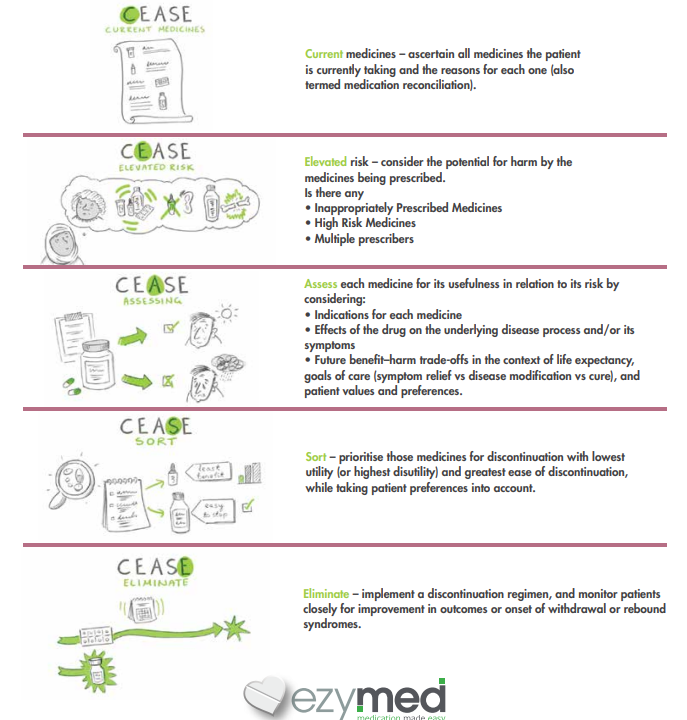
Deprescribing
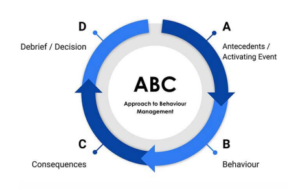
Regular review of the drug treatment of chronic non-cancer pain is recommended. Assess the effectiveness of analgesia using the ‘5As’ principle:
- Analgesia
- Activity
- Affect
- Adverse Effects
- Aberrant behaviours, such as unapproved increase of dose or use of the drug to treat other symptoms.
Consider deprescribing if there has been no meaningful improvement in function or pain, when the risk of harm (side effects) outweighs the benefit, and/or if the resident reports no pain for more than 3 months.
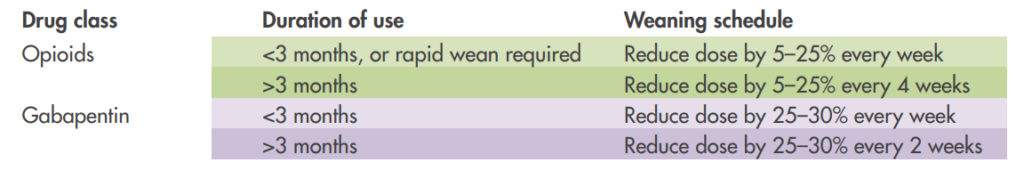
Doses should be reduced slowly to avoid rebound side effects and possible signs of dependence.
General Approach For Weaning Opioids And Gabapentinoids
Conclusion
Managing chronic non-cancer pain, especially in frail older people, remains challenging. The altered harm versus benefit profiles of drugs in this group of patients needs to be carefully considered and regularly reviewed when prescribing. If pain remains troublesome despite standard therapies, consideration should be given to seeking support from a geriatrician, pain specialist, or pain service.
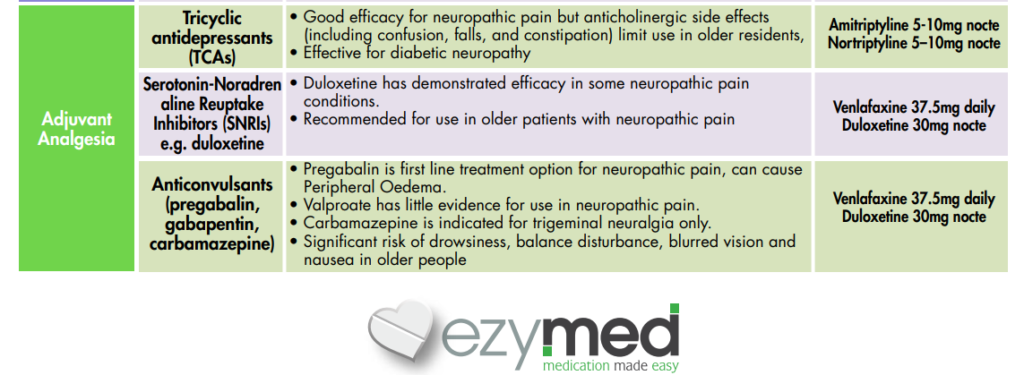
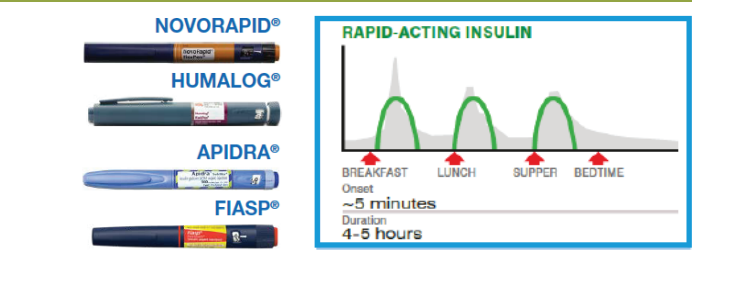
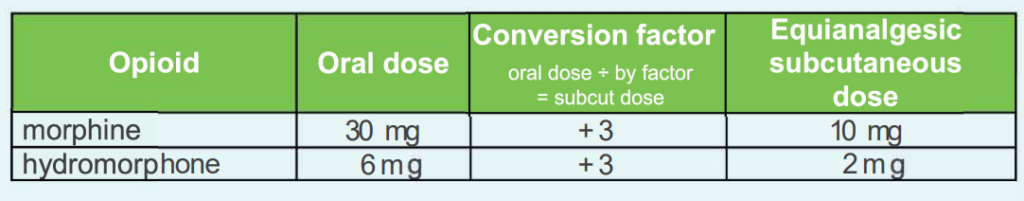
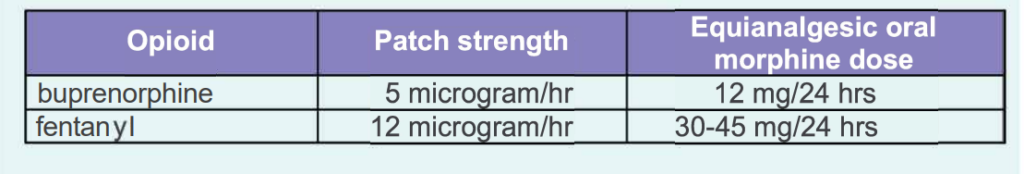
Opiod Conversion Guide
These conversions are a guide only. Patients may vary in their response to different opioids. After changing opioids, close assessment should follow and the dose altered as necessary.
Equianalgesic doses of oral opioids
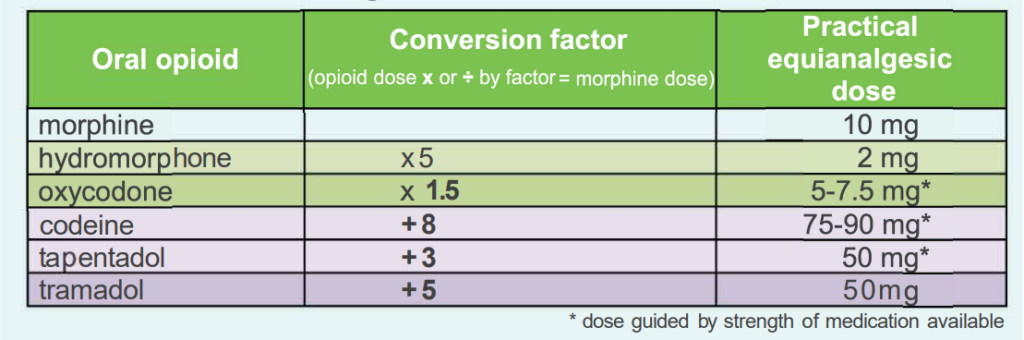
• GREEN shaded opioids are those STRONGER than morphine mg for mg
• PURPLE shaded opioids are those WEAKER than morphine mg for mg
Subcutaneous route conversions
Transdermal preparation conversions
Methadone and medicinal cannabis conversions are complicated and prescribing should be restricted to medical specialists for pain management.
• Reduce Opioid dose by 30-50% to accommodate for unknown cross-tolerance and titrate to goal
• Short acting PRN opioid doses are approximately 10-20% of total 24hr scheduled opioid dose.
online Opioid Calculator – http://www.opioidcalculator.com.au/opioidsource.html

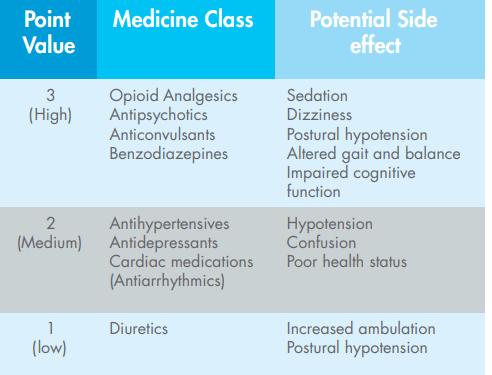
Pain Management – Summary of Medications