The National Aged Care Mandatory Quality Indicator Program started in 2019. From July 2021, there will be two new quality indicators (QIs) that Aged Care Providers will have to report on:
• Falls and major injury
• Medication management
What is required within the Quality Indicators on Medication Management?
The Medication Management QI covers two issues:
• Polypharmacy – defined as the prescription of nine or more medications to a care recipient
• Antipsychotic medications – Care recipients assessed for antipsychotic medications and care recipients who received an antipsychotic medication for a diagnosed condition of
psychosis
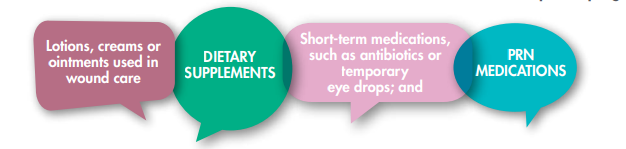
What is not counted in Polypharmacy Reports?
Any medication with an active ingredient is counted in the polypharmacy quality indicator, except
for those listed below which should not be included in the count of medications as per the QI program:
“Different dosages of the same medicine is also NOT to be counted as different medications.”
Is Polypharmacy an issue in aged care?
We know that 2 out of 3 Australians aged over 75 take 5 or more medicines and in residential aged care homes, residents are taking on average 9 to 10 medicines each day. Polypharmacy has demonstrated a major impact on the health and financials of an older person. It can affect how they feel, their ability to enjoy daily activities and how they interact with their family, other residents, and carers. The elderly taking 5+ medicines have a higher risk of
• Side effects: Interactions with medicines
• Adverse outcomes include: falls, increased frailty, hospitalisation, and overall mortality.
Polypharmacy can also lead to additional nursing and administrative time; time they would often prefer to spend doing more enjoyable activities with the older person.
What are the causes of Polypharmacy?
There are many factors that may contribute to the development of polypharmacy:
• More medicines on the market • The use of medicines to alleviate symptoms • Multiple chronic conditions
• Longer lifespans • Multiple prescribers • Complex care needs • Reluctance to trial ceasing medicines
• Use of regular rather than PRN dosing
Polypharmacy can also increase the risk of the Drug Burden Index, but what is a Drug Burden Index? It is defined as the functional burden of medications in older people.
Older people carry a high burden of illness for which medications are indicated, along with an increased
risk of adverse drug reactions. The drug burden index was developed to determine the drug burden based on
pharmacological principles in relation to physical and cognitive performance apart from the underlying disease
indication.
Examples of medications that contribute to the Drug Burden Index –
| MEDICATION | CAUTION |
| Non-steroidal anti-inflammatories e.g. naproxen, ibuprofen | Risks: Gastrointestinal bleeding, cardiac failure, nephrotoxic. Suggested action: Avoid where possible. If essential, offer short courses with proton pump inhibitor cover. |
| Hypnotics e.g. benzodiazepines | Risks: Drowsiness, confusion, poor balance and increased risk of falls. Suggested action: Avoid where possible oroffer short course only |
| Diuretics e.g. furosemide | Risks: Hypotension, increased risk of falls, nephrotoxic, Diuresis can be difficult for patients with poor mobility. Suggested action: Review renal function regularly and ensure good hydration status. |
| Anti-chlolinergics e.g. tricyclic antidepressants, antihistamines, oxybutymin |
Risks: Postural hypotension, dizziness, increased falls, urinary retention, constipation and confusion. Associated with risk of dementia. Suggested action: Stop where possible and consider alternative. |
| Antidepressants, e.g. tricyclics, selective sertonin reuptake inhibitors (SSRI) |
Risks: Confusion, dizziness, hypnatraemia and falls. May be toxic in overdose. Can be cardiotoxic and increased risk of stroke and heart attack. Suggested action: If necessary, opt for SSRI. |
| Hypoglycaemic diabetic medication e.g. sulfonylureas |
Risks: Hypoglycaemia. Suggested action: Target HbA1c of 7.5% or 58 mmol/mol if life expectancy less than 10 years. |
Anti-coagulants |
Risks: Warfarin interacts with many drugs and foods. Suggested action: Careful counselling and consider risk of falls |
| Cardiac glycosides e.g. digoxin | Risks: Caution in renal impairment as increased risk of toxicity. Suggested action: Start with lower doses in the elderly. Monitor renal function. |
Anti-psychotics |
Risks: Cognitive impairment, sedation, cardiac arrhythmias, parkinsonism, increased risk of stroke and heart attack, osteoporosis. Suggested action: If used for a mental health disorder, review regularly. Avoid for behavioral disturbance in dementia. |
Other resources recommended when reviewing medication in the elderly include –
• Beers criteria – Potentially Inappropriate Medicines (PIMs) –
• STOPP/START criteria – looking at the Potential Prescribing Omission (PPO) when starting ANY new medicine.
• MATCH-D criteria – Medication Appropriateness for comorbid health conditions in Dementia patients
What happens during a Residential Medication Management Review?
What happens during a Residential Medication Management Review?

Our Ezymed pharmacists have been clinically trained and certified to conduct Residential Medication Management Reviews.
The Clinical pharmacist reviews typically focus on –
• Why is the medicine being taken? Is it for preventative or symptomatic treatment?
• Is the medicine appropriate for the consumer?
• Is it still needed?
• Can the dose be reduced or discontinued?
• How many medicines are being taken overall?
• What is their drug burden?
• Would the consumer benefit from the reduction of any of them?
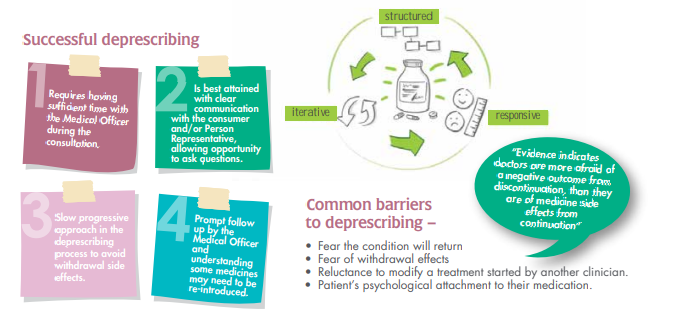
Deprescribing, is it possible in aged clients?

Deprescribing has been defined as, “the process of withdrawal of an inappropriate medication, supervised by a health care professional
with the goal of managing polypharmacy and improving outcomes”.
Br J Clin Pharmacol. 2015 Dec;80(6):1254-68
Deprescribing should always be part of the holistic medication review
for all patients, particularly the vulnerable elderly.
Structured deprescribing can successfully reduce the number of medicines by 1-3 medicines per person
Clinical trials on Deprescribing
Medication Withdrawal Trials in people aged 65 years and older: A systematic review of 31 clinical trials in older people
concluded that specific classes of medications like Antihypertensives, Benzodiazepines, and Psychotropic drugs could be withdrawn successfully without causing harm in people aged 65 years and older.
The War against Polypharmacy: a new Cost-effective geriatric approach to improving drug therapy in disabled elderly
people: Evaluations of the use of medications in 190 geriatric patients led to discontinuation of 322 drugs in 119 patients with no significant adverse effects after 12 months. Drugs discontinued no adverse effects including NSAIDs, analgesics, statins, oral hypoglycemics, carbamazepine, and digoxin.
Did you know that consumer reluctance/refusal to take medicines should be considered as a prompt to consider deprescribing, rather than changing dosage forms or finding alternate ways to administer the medicines?
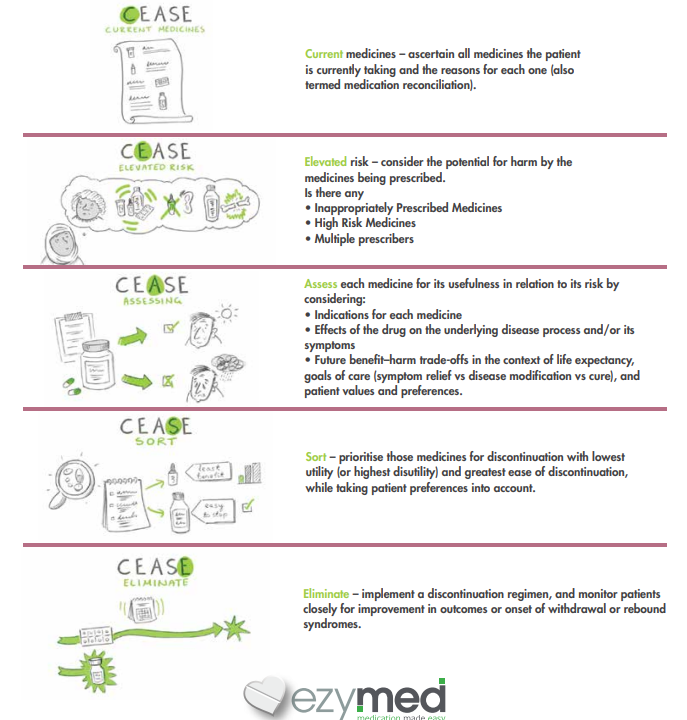
A Patient-Centred Medication Review is the answer to effective deprescribing The CEASE Framework was developed to assist in the development of an effective care plan when deprescribing –