High-Risk Medicines are those that have a high risk of causing injury or harm if they are misused or used in error. Error rates with these medications are not necessarily higher than with any other medicines, but when problems occur, the consequences can be more significant.
The National Safety and Quality Health Service (NSQHS) Standard on Medication Safety requires health services to identify High-Risk Medications used within the organisation and take appropriate action to ensure they are stored, prescribed, dispensed, and administered safely. As a minimum, facility policy on High-Risk Medicines should include Hydromorphone, Oral Methotrexate, Paracetamol dosing, and Anticoagulants.
High-Risk Medicines can also include
• Medicines with a narrow therapeutic index such as Digoxin, Lithium, and Warfarin.
• Medicines that present a high risk when administered via the wrong route.
• Have similar names.o
• Administered as variable dose daily, weekly or monthly.
There is no standard list ofhigh-risk medicines for aged care homes in Australia, however, lists have been created largely based on incident reporting systems in different health services, jurisdictions and countries.
Some Recommended requirements when discussing High-Risk Medicines –
1. Establish a policy within your organisation for the management of High Risk Medicines including a list of medicines you consider as high risk.
a. Assess and determine the medicines to be included in the register.
b. Maintaining regular updates and reviews of the register.
c. Establish protocols for each category of High Risk Medicine.
d. Incident reports on policy compliance and corrective action needed for High-Risk Medicines.
2. Protocols for managing residents on High Risk Medicines should include:
a. Responsibilities for the prescribing and administration of high-risk medicines.
b. Additional considerations for patients with conditions that may affect drug excretion such as renal function and weight.
c. Patient monitoring parameters, for example, clinical observations, are required to ensure a timely response to adverse events such as sedation and breathing rate side-effects associated with the treatment.
d. Therapeutic drug monitoring requirements, including laboratory tests and dose amendment.
e. Specific storage requirements to minimise selection error.
f. Timeframe for review of parameters and person responsible.
g. Potential risk of inappropriate use of these medicines
3. Establish strategies to minimise the risk with High-risk Medicines using measures such as:
a. Pre-measured medicine doses in a form that requires minimal manipulation prior to administration (blister packs or sachets).
b. Use of shelf reminders, Checklists, and alerts placed within the treatment room and/or electronic system in use.
c. Review of incidents or near-misses to reassess systems in place.
It is important to note that a single risk-reduction strategy for a High-Risk Medicine is rarely capable of preventing patient harm. When seeking to reduce the likelihood of harm in healthcare settings, a range of strategies need to be considered to promote safer use or decrease the opportunity for misuse or error. Risk-reduction strategies can be based on a review of how High-Risk Medicines are managed within the organisation using audits, incident analysis, risk assessment tools, and benchmarking activities.
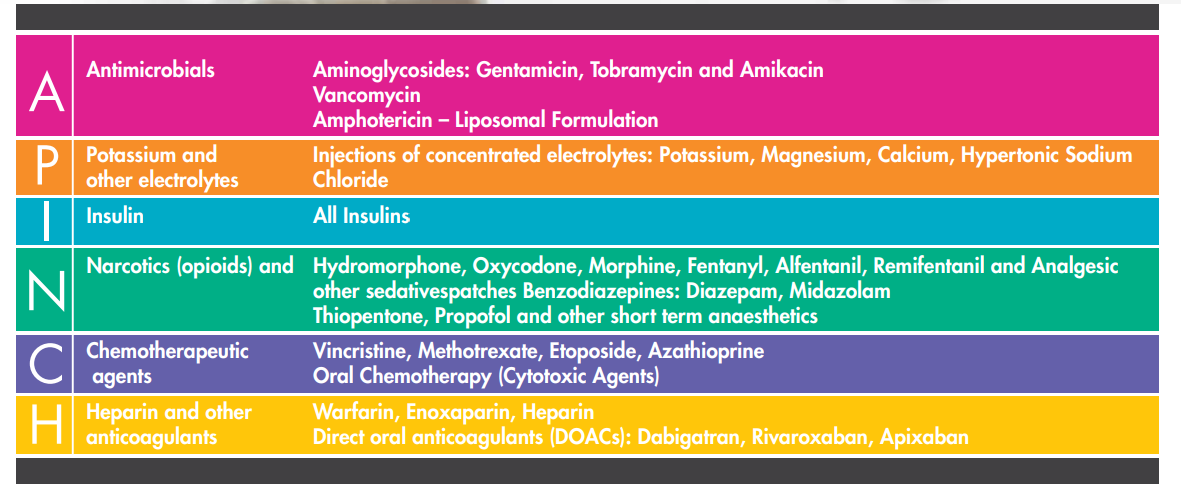
In the acute sector, the ‘APINCH’ acronym and classification are widely used to assist clinicians to focus on a group of medicines known to be associated with a high potential for medication-related harm. The ‘APINCH’ classification is not an exhaustive list and other medicines or classes of medicines may also present a high risk and may be included alongside the APINCH list within your organisation, examples include Digoxin, Paracetamol, and oral
hypoglycaemics.
Possible reporting systems from Ezymed that can assist in such activities may include:
• Automated list of residents on High Risk Medicines using the
‘APINCH’ criteria.
• Assist in protocols for prescribing and administering
High Risk Medicines.
• Review of incidents and near-misses during MAC and adopting
strategies to minimise risk with High-Risk Medicines
A for Antimicrobials
Injectable antibiotics such as Aminoglycosides and Vancomycin are the typical High-Risk Medicines in this category and are most encountered in hospital settings.
Enhanced awareness and vigilance regarding the supply of these medicines see them to be less likely reported in an incident.
A more common cause for a significant consequence in aged care is the supply of an antibiotic to which a patient is allergic.
While there is a greater awareness of determining the nature of a previously reported antibiotic allergy, caution is still warranted, and appropriate history taking, and
counseling should always be provided when supplying medicines from this group.
A retrial of an antibiotic in someone with a history of an allergic reaction should be done in an acute care setting and not recommended in an aged care home.
P for Potassium and other Electrolytes
Injections of Potassium, Magnesium, Calcium, Hypertonic Sodium Chloride.
Although, the concentrated electrolytes are less likely to be encountered except in acute hospital settings, some pharmacists and pharmacy staff have in some cases
misunderstood requests for an oral potassium supplement and inadvertently supplied potassium permanganate, Condy’s Crystals, not recommended for oral administration
where the client dissolved an amount of Condy’s Crystals and consumed the chemical leading to hospitalisation.
Note – Condy’s Crystals (Potassium Permanganate) commonly used as salt crystals in baths for the treatment of infected eczema when there are blisters, pus and/or oozing
I for Insulins
Although all insulin types are recommended to be part of the High-Risk Medication list, the most commonly reported error involved mixing-up between NovoRapid and NovoMix and RNs not knowing short-acting from long-acting Insulin.
In a relatable case scenario: an older patient with type 2 diabetes was prescribed NovoMix in the morning. NovoRapid was supplied and administered for some weeks, leading to several episodes of hypoglycaemia and ultimately, a fall that lead to hospitalisation due to a fracture
N for Narcotics and otherSedatives
All aged care clinicians are aware of the risks associated with these medicines, especially when more than one drug is being taken or when taken in combination with
sedatives/psychotropics and other comorbidities.
Drugs of higher risk such as Fentanyl, Pethidine, Methadone, and Hydromorphone require particular care and should always be treated with the utmost caution.
Classes such as antipsychotics, anxiolytics, and antiepileptics have been considered in this category of high risk medications.
We all have a duty of care – independent of that of prescribers – to ensure the medicines are taken in a way that is both safe and efficacious.
While the introduction of regular monitoring using the Psychotropic Self-assessment forms will help aged care facilities and prescribers to deal with the challenges around these medicines, ongoing vigilance and clinical consideration remains necessary.
Increased hospitalisation and mortality in the community has been linked to early supply of medicines including narcotics, benzodiazepines or Z-drugs. Likewise, in aged care it has been linked to multiple supplies of Opioids, sedatives and/or antipsychotics dispensed from an incomplete Medication Chart or Medication order
C for Chemotherapeutics Agents
Cytotoxic medications are of concern in aged care homes as these medicines and their consumers need to be managed with added care and ALWAYS be treated as High Risk Medicines by the prescribers.
Please note this does not apply to Hazardous, non-cytotoxic, medicines.
Common factors to consider in all patients prescribed Cytotoxics, even those who have been taking the medicine for some time include –
• advancing age • significant weight loss • decline in hepatic or renal function and • other medicines prescribed.
All of which have the potential to impact on the safety of chemotherapeutics.
A case scenario in an aged care home involving daily dosing of Methotrexate due to incorrectly labeled items from their local pharmacy.
It is particularly concerning when methotrexate is required to be administered by non-RNs in DAAs not adequately labeled with appropriate warnings or packed in the same blister or sachet as other medications, making checking harder.
It is strongly recommended that all packing of Cytotoxics is made into separate blister packs or sachets, with this packaging marked as containing a cytotoxic.
H for Heparin (and other anticoagulants)
With the growing use of direct oral anticoagulants (DOAC), we have seen a rise in the number of incidents reported due to the range of indications, dose variations, and the need for dose adjustment in certain patient groups has led to an increased risk of error or incident and hospitalisations.
While the benefits are apparent for the absence of regular monitoring in the DOACs, this has led to a degree of complacence on the part of the health care team leading to this class of medicines as being of lower risk. Incidents linked to DOACs have involved:
• the wrong strength being supplied – such as Dabigatran 150mg instead of 100mg or Rivaroxaban 20mg instead of 15mg.
• Wrong frequencies – such as Rivaroxaban twice instead of once daily,
• omissions of the drug from blister packs / DAAs by supply pharmacies, or
• the client taking a DOAC independently while also receiving it in a DAA.
Other anticoagulants such as the Low Molecular Weight Heparins and Warfarin still feature in this group of High-Risk Medicines and continue to have their own incidents
however, more stringent measures in aged care homes have seen close review and follow-up of all incidents reducing the need for hospitalisation
Other High-Risk Medications to Consider in Residential Aged Care Homes
TRANSDERMAL PATCHES:
• Confirmation from the prescriber should be sought if multiple patches are to be applied.
• The time of application, site of
application, and time of removal should be documented on a separate administration chart.
• Transdermal patches should not be
exposed to extremes temperature.
• Transdermal patches should not be cut.
• Transdermal patches containing opioids should be securely disposed of, for example, in sharps bin
PARACETAMOL ORDERS:
• PRN orders to indicate on the directions that resident is on REGULAR Paracetamol dose and calculate maximum daily dose accordingly.
• Patients weighing <50kg must have their daily Paracetamol dose reviewed. Please note o Weight range 40-50kg, recommended daily Paracetamol dose is 2500mg – 3000mg per day (in 3-4 divided doses) o Weight range 30-40kg, recommended daily Paracetamol dose 1800mg – 2500mg per day (in 3-4 divided doses)
INJECTABLE ORDERS:
(apart from Insulin)
• The day/date for administration must be clearly displayed on the chart,
• Should clearly state for “RN only”
administration,
• The order must indicate if the injectable is for IMI orSubcutaneous,
• Stock should be available for day of administration with a prompt for
administration from the electronic
singing software or signing sheets
supplied from the pharmacy,
• Administration signing section should be blocked out for all other days.
Next time you are doing a medication round and have to crush medicines, administer Warfarin, Insulin, Oxycodone and/or a patch prescribed for your resident, consider the potential danger that even ‘APINCH’ can do.
How To Reduce The Risks
By the RACF
• Access to pre-packed medicines by your pharmacy in DAAs for high-risk medicines as much as possible.
• Use of checklists, alerts, and information technology systems, to assist administering staff in identifying High-Risk Medicines.
• Patient weight and swallowing ability documented on the medication chart, and reviewed by RNs regularly.
• Regular review of incidents to assess the systems in place.
• Medication review (request RMMR) prioritising patients on High-Risk Medicines. By the Prescriber
• Rout of administration clearly identified. The use of multiple routes of administration in the one order should be avoided, eg. Maxolon IMI/Oral.
• Strength of medicine and dose to be administered clearly visible in dose units or dose per volume of liquid, eg. Panadol 250mg/5ml, 10mls (500mg) TDS.
• Indication to be completed on the medication chart for all High-Risk Medicines.
• Variable dose orders to have the day of the week or date of the month for administration CLEARLY documented on the chart, eg. Methotrexate 10mg, 3 tablets mane on WEDNESDAY
High-Risk Medicines for monitoring recommended by Ezymed
1. Antimicrobial – Long-term use of any Antimicrobials (charted for > 4 weeks)
2. Paracetamol –
Residents on combined orders of regular and PRN, residents with weight range <50Kg.
3. Insulin –
Residents on any Insulin
4. Narcotic Opioids –
Residents on patches and multiple strengths or forms of Opioids (>2)
5. Chemotherapeutic agents –
Cytotoxic drugs excluding hormonal antineoplastics)
6. Heparin and oral anticoagulants –
Oral – Warfarin, Dabigatran, Rivaroxaban and Apixaban. Injectable – Enoxaprin and Heparin.
7. Sensitive Drugs –
Drugs with a narrow therapeutic index including Digoxin, Thyroxine, Dilantin, Perhexilin, Lithium, Valproate, and Warfarin


