Diabetes in the Elderly
Around one-quarter of all people living in residential aged care facilities (RACFs) have diabetes. These people may have lived with the condition for many years and may be living with
comorbidities and diabetes-related complications, particularly with insulin management. As a result, care is often complex.
● For older people living in residential aged care, helping them maintain the best quality of life should be the main principle of diabetes management.
● Monitoring blood glucose levels is one way to do this, but it is just part of an overall management plan. Diabetes care requires a balance between healthy eating, physical activity and medicines, such as tablets and/or insulin. Stress, illness and other comorbidities can also have an effect on a resident’s diabetes.
Diabetes Management in Aged Care
● Diabetes management in aged care aims to increase knowledge and awareness of diabetes in older people for staff who support those living with diabetes in RACFs this can be accessed as a resource from our online portal.
● Residents in aged care are more likely to be frail with reduced life expectancy. A significant proportion of them may have cognitive impairment or dementia, with reduced capacity to communicate how they are feeling. The ability of staff to recognize and respond in a timely manner has an enormous impact on residents’ quality of life.
● Certain policies and procedures must be in place in residential care facilities for consumers with diabetes. Some of the recommended tools are available from ndss.com.au (Quality review tool: management of residents who have diabetes) to assist in the overall assessment and quality of the management and care of consumers diagnosed with diabetes in your facility and consistent with the Aged Care Quality Standards
They include:

- ADMISSION AND SCREENING
- DIABETES MANAGEMENT CARE PLAN
- HYPOGLYCAEMIA
- HYPERGLYCEMIA & SICK DAY MANAGEMENT
- COMPLICATIONS SCREENING AND PREVENTION TOOL
- STAFF TRAINING
- FACILITY SUPPLIES, EQUIPMENT, and MAINTENANCE
Insulin Management in Aged Care
Insulin is a hormone produced by beta cells in the pancreas. It works by allowing glucose to move from the bloodstream and into cells for energy and controlling the release of glucose from the liver.
● For all people with type 1 diabetes injecting insulin is essential and should never be stopped. Some people with type 2 diabetes will require insulin injections as their condition progresses.
● Insulin is a high-risk medicine with significant dangers if administered inappropriately. It can’t be taken orally, via tablets or capsules. It must be given using a needle, insulin pen device, or pump.
● There are different types of insulin, including rapid-acting, short-acting, intermediate-acting, long-acting, and pre-mixed insulin.
● Depending on the resident and type of insulin and insulin-giving device being used, the insulin may be given once a day or several times a day, depending on their needs.
● Insulin works best when it’s injected into the fatty layer just beneath the skin and above the muscle. It’s recommended that insulin is injected into the abdomen (tummy). In some cases, the thigh or buttocks may be used. The length of the needle is important as it needs to penetrate the skin
When administering insulin, you should:
✓ the right dose and BGL range
✓ Use a new needle every time
✓ Check you are giving the right type and dose of insulin
✓ Prime the needle every time to remove
air and start the flow of insulin (also known as an “air shot”)
✓ Insert the needle at 90 degrees (a right
angle) unless advised otherwise by your health professional
✓ After injecting the insulin, hold the needle under the skin for 10 seconds to make sure you get the full dose
✓ Rotate injection sites so that you use a different site every time to avoid
developing fatty lumps
✓ If using an insulin pen, remove the
needle from the pen after each injection
✓ Dispose of all sharps safely
Storing insulin:
● Store your unopened insulin in the fridge (away from the freezer/chiller section). Don’t let your insulin freeze.
● Keep the insulin you are using at room temperature (below 25 degrees celsius). Once insulin has been opened, it can stay at this temperature for up to 28 days.
● It’s fine to keep the current insulin pen in your medication trolley or resident’s cupboard. Don’t keep it in a place where it might get hot, like the car or near a window.
● Once open, dispose of after 28 days
DO NOT
✗ Use the insulin after the expiry date
✗ Use the insulin if it doesn’t look the way it should, or if it has been frozen or exposed to extreme heat
✗ Shake the insulin too hard
✗ Inject in areas where there are scars, stretch marks, or lumps
✗ Inject through clothes
Monitoring blood glucose – BGL
How is blood glucose monitored?
glucose meter and a finger prick to get a ‘snapshot’
of what a resident’s glucose level is at a specific point
in time
Target BGL 6–15 mmol
ordered 2 to 4 times a year. The result reflects an
average blood glucose level for the last 2 to 3
months
HbA1c<6% is associated with falls
How to Calculate or Adjust the dose of Insulin? (suggested Algorithm)
| Lowest BGL over previous 3 days ( fasting or pre-prandial)* <10 8-10 7-7.9 6-6.9 4-5.9 <4.0 or severe hypoglycaemic event ✝ |
Adjust insulin dose once or twice weekly to achieve the target BGL 1 by 4 units 1 by 2 units No change No change ⬇by 2 units ⬇by 4 units |
*Adjustment should be based on the lowest BGL over the previous 3 days.
✝ Hypoglycaemia should prompt a review of other oral therapy as well which insulin is adjusted will depend on the regimen and the target glucose. The algorithm can be used for both basal and premixed insulin titration
Types of insulin:
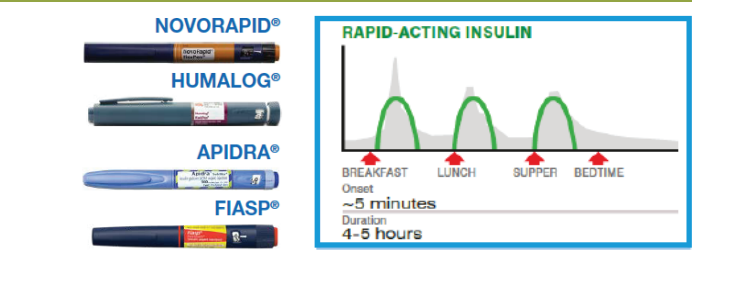
Bolus insulin: Ultra-short ActingGiven before meals or for correction of blood glucose levels
● Clear solution
● Rapid-acting insulins must be given at mealtime, no more than 15 minutes before a resident starts eating.
● Has a peak action 1-1.5 hours after being injected and continues to lower blood glucose levels for 3-5 hours.
● Fiasp must be given during or immediately after the meal as it starts to work within 5-15 minutes with a peak action 0.5-1.5 hours after being injected and continues to lower blood glucose levels for 3-5 hours
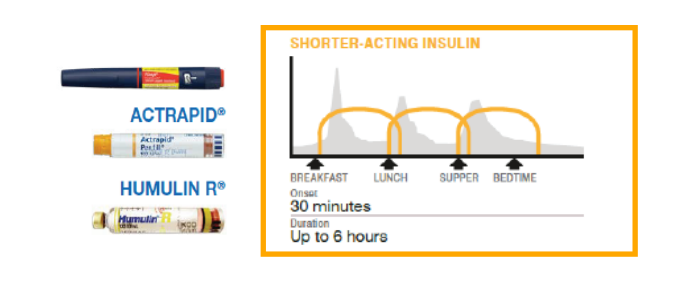
Bolus insulin: Short Acting
Given before meals or for correction of blood glucose levels.
● Clear solution
● Starts to work about 30 minutes after injecting
● It is important to eat within 30 minutes of injecting the insulin
● Given as a bolus dose to keep your glucose levels within your target range after a meal
● Has a peak action 2-3 hours after being injected and continues to lower blood glucose levels for 6-8 hours.
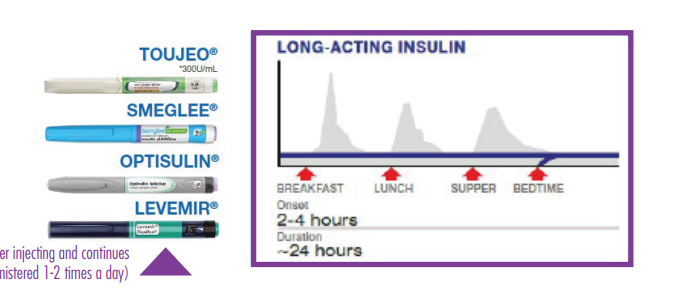
Basal insulin (Background Insulin): Long-acting
Used to control fasting glucose levels (between meals).
● Clear solution
● Injected once daily at the same time each day
● Starts to work within 1-2 hours (1-6 hours for Toujeo) after injecting
● Has no peak action and continues to lower blood glucose levels for 24 hours (24-36 hours for Toujeo).
( Levemir is the ONLY long-acting that has a peak action in 6-8 hours after injecting and continues to lower blood glucose levels for 12-24 hours. (usually administered 1-2 times a day )
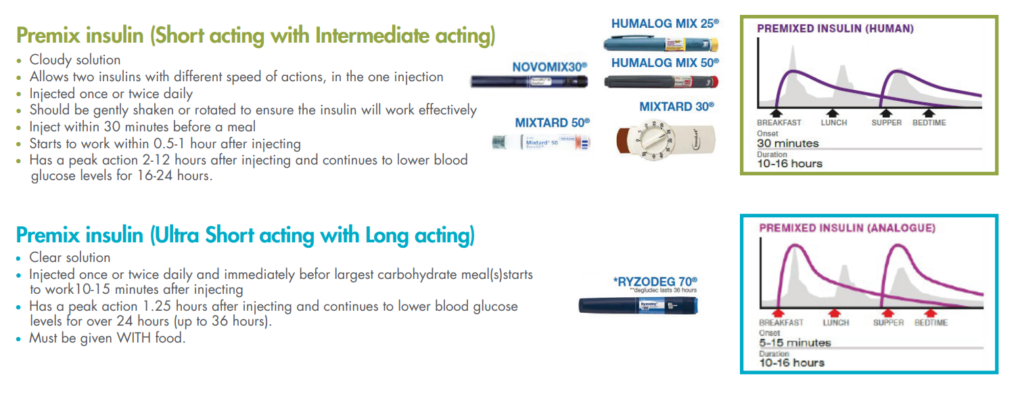

Changing Insulins
● When switching from twice-daily human isophane insulin (e.g. Humulin) to once-daily insulin glargine (e.g. Toujeo), the daily dose is usually reduced (by about 20%) initially and then adjusted according to the response.
● When switching from another mixed insulin regimen to the insulin degludec
(Ryzodeg) with insulin aspart combination:
● In type 2 diabetes, use the previous total daily insulin dose
● In type 1 diabetes, start with 60–70% of the previous total daily dose together with a short- or ultra-short-acting insulin at other meals
● Adjust dose according to individual response
Target Blood Glucose 6–15 mmol/L
THE PRIMARY AIM IS TO AVOID HYPOGLYCAEMIA AND THE SYMPTOMS OF HYPERGLYCAEMIA.
The McKellar Guidelines for Managing Older People in Residential and Other Care Settings recommend –
● low blood glucose (hypoglycaemia) is regarded as generally less than 6 mmol/L, especially in frail older people, and
● too high blood glucose(hyperglycaemia) generally occurs when blood glucose is greater than 15mmol/L, especially if it’s consistently above 15 mmol/L.
● HbA1c should be monitored every 6-12 months and the target should be generally 7-8% and up to 8.5% in patients with dementia.
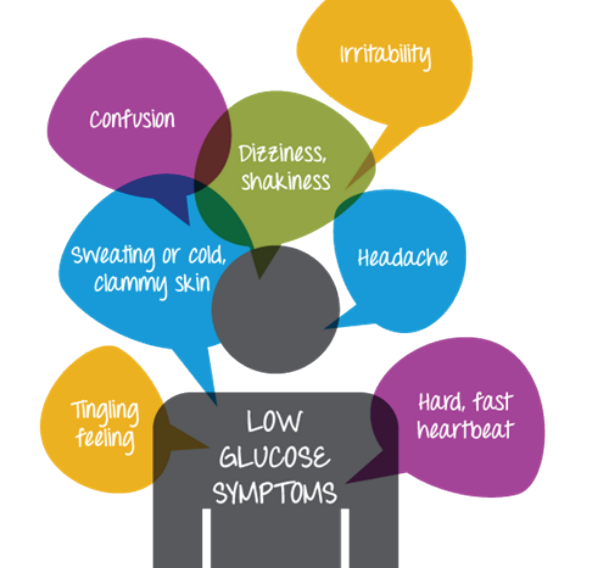
HYPOglycemia
Is defined as low blood glucose levels. BGL < 6mmol/L
Can happen for a variety of reasons, but commonly due to the imbalance between food and Diabetic medication, unplanned exercise, and/or alcohol. The signs and symptoms can be
● Neuroglycopenic – characterized by impairment of cognitive function, irritation or aggressive behavior,
OR
● Autonomic – involving the Sympathetic and
parasympathetic systems “fight or flight” type of reaction.
If Hypoglycemia is untreated,
the individual can become increasingly
confused and eventually
lose consciousnesses.

HYPERglycaemia
When the blood glucose level (BGL) > 15mmol/L.
Often happens slowly but it can also happen suddenly, depending on the cause. What are the possible causes of high blood glucose?
● infection/illness
● not enough, or missed insulin or other diabetes medicines
● greater than usual food intake (carbohydrates)
● medications used to treat other illnesses, for example, steroids and antipsychotics
● emotional stress or pain
● undiagnosed diabetes
A high BGL every now and then is not a problem.
However, action should be taken if the reason for the resident’s high BGL is unknown;
if they have had high BGLs for several days; or if they have symptoms of hyperglycemia.

Action Plan for Hyperglycemia in Aged Car
✓ Implement sick daycare if indicated (see the next section).
✓ Arrange a medicines review if hyperglycemia persists.
✓ Consult with the doctor for laboratory and other diagnostic investigations.
✓ Consider referral to a dietitian.
RESIDENT SICK DAY PLAN – All residents with diabetes should have a sick day plan.
Always refer to resident’s diabetes care plan
Being sick can make things more difficult for a resident with diabetes. The illness might cause their blood glucose levels to rise, and it might also make it harder to manage their diabetes.
How diabetes is managed during an illness depends on whether the resident has type 1 or type 2 diabetes. Residents may need more frequent blood glucose monitoring and more insulin (if they usually take insulin).
Note – Never stop all Insulin, but you may need to stop oral tablets if ketones are present If a resident is sick their blood glucose levels (BGLs) may increase or decrease.
When to initiate the Sick Day Action Plan?
● there is a notable change: feeling weak, drowsy, anxious, irritable, tired, sleepy
● there are signs of fever or infection (chest, urinary, skin)
● diarrhoea or vomiting
● changes in appetite (hungry, thirsty or loss of appetite or poor intake of food)
● new or increased pain

ASSESSING THE RESIDENT
Do a BGL
(is it high or low per resident’s
diabetes care plan?)
Note clinical signs such as:
● increase/decrease in temperature,
change in breathing rate (laboured,
increased)
● increased heart rate, sweaty
● signs of dehydration e.g. skin turgor,
hypotension, dry mouth, low urine output
● Notify GP
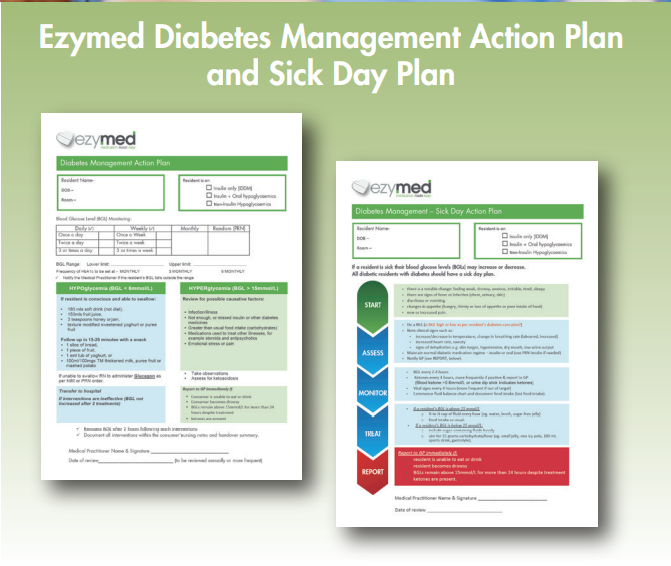
MONITORING recommendation
● BGL every 2-4 hours
● ketones every 4 hours (more frequently if
positive & report to GP)
● vital signs every 4 hours (more frequent if out of target)
● commence fluid balance chart
● document food intake (last food intake
TREATMENT recommendations
If a resident’s BGL is ABOVE 15 mmol/L:
● ¼ to ½ cup of fluid every hour (for example water, broth, sugar-free jelly)
● food intake as usual.
If a resident’s BGL is BELOW 15 mmol/L:
include sugar-containing fluids hourly –aim for 15 grams carbohydrate/hour (for example, small jelly, one icy pole, 100 mL sports drink, gastrolyte).


